Headaches and hormones: What's the connection?
Headaches and hormones: What's the connection?
Being female has some real health advantages, but not when it comes to headaches — particularly migraines. Fortunately, there's help.
Many factors contribute to headaches for both men and women, including family history and age. Women, however, often notice a relationship between headaches and hormonal changes.
The hormones estrogen (ES-truh-jen) and progesterone (pro-JES-tuh-rohn) play key roles in regulating the menstrual cycle and pregnancy and may also affect headache-related chemicals in the brain.
Having steady estrogen levels may improve headaches, while experiencing estrogen levels that dip or change can make headaches worse.
Though fluctuating hormone levels can influence headache patterns, you're not completely at the mercy of your hormones. Your doctor can help you treat — or prevent — hormone-related headaches.
During menstruation
Your menstrual-related migraines may be treated in several ways. Proven treatments for migraine are often effective for treating menstrual migraine. They include:
- Apply ice. Hold a cold cloth or an ice pack to the painful area on your head or neck. Wrap the ice pack in a towel to protect your skin.
- Relaxation exercises. Try relaxation exercises to lower stress.
- Biofeedback. Biofeedback may improve your headaches by helping you to monitor how your body responds to stress.
- Acupuncture. Acupuncture may improve your headaches and help you relax.
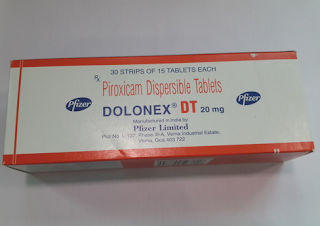
- Take over-the-counter pain relievers. Your doctor may recommend you take nonsteroidal anti-inflammatory drugs (NSAIDs), such as naproxen (Aleve) or ibuprofen (Advil, Motrin IB, others). These medications may relieve your pain soon after your headache begins.
- Take triptans. Your doctor may prescribe triptans, medications that block pain signals in your brain. Triptans often may relieve pain from your headache within two hours and help to control vomiting.
- Take pain relievers and triptans. Some women may take a combination of NSAIDs and triptans to relieve pain from menstrual migraines.
- Take other prescription pain medications. Sometimes your doctor may suggest other prescription pain medications, such as dihydroergotamine (Dihydroergotamine Mesylate).
Preventive treatment
If your menstrual cycle is regular, it's often most effective to take preventive headache medication starting a few days before your period and continuing through up to two weeks after the start of your period.
If you have migraines throughout your menstrual cycle or you have irregular periods, your doctor may recommend that you take preventive medications every day.
Daily medications may include beta blockers, anticonvulsants, calcium channel blockers, antidepressants or magnesium. Doctors will review any other medical conditions you may have to determine which medications may be most appropriate for you.
Making lifestyle changes, such as reducing stress and exercising regularly, also may help reduce the frequency, length and severity of migraines.
Hormonal contraception use
For some, hormonal contraception may help reduce the frequency and severity of menstrual-related migraines. It works by minimizing the drop in estrogen associated with the menstrual cycle.
Using hormonal contraception to prevent menstrual-related migraines may be appropriate for women who haven't been helped by other methods.
Other women may first experience migraines while using hormonal contraception. If you experience migraines while using hormonal contraception, talk to your doctor.
It may help to:
- Use a monthly birth control pill pack with fewer inactive (placebo) days.
- Eliminate the placebo days completely from most months by taking extended-cycle estrogen-progestin birth control pills (Seasonale, Seasonique, others).
- Use birth control pills that have a lower dose of estrogen to reduce the drop in estrogen during the placebo days.
- Take NSAIDs and triptans during the placebo days.
- Take a low dose of estrogen pills or wear an estrogen patch during the placebo days.
- Use an estrogen-containing skin patch during the placebo days if you're using a birth control patch.
- Take a progestin-only birth control pill (Micronor, others) as an alternative to oral estrogen-progestin birth control pills, if you're not able to take estrogen-progestin birth control pills due to other conditions.
During pregnancy
If you experience chronic headaches, discuss medications and therapies that can help you during pregnancy with your doctor before you become pregnant. Many headache medications may have harmful or unknown effects on a developing baby.
After delivery, an abrupt decrease in estrogen levels — along with stress, irregular eating habits and lack of sleep — may trigger headaches again.
Although you'll need to be cautious about which headache medications you take while you're breast-feeding, you'll likely have more options than you did during pregnancy. Your doctor can tell you which medications you may take while you're breast-feeding.
During perimenopause and menopause
For some women, migraines improve once their menstrual periods cease, but tension headaches often get worse. If your headaches persist after menopause, you often can continue to take your medications and use other therapies.
Hormone replacement therapy, which is sometimes used to treat perimenopause and menopause, may worsen headaches in some women, improve headaches in others or cause no changes. If you're taking hormone replacement therapy, your doctor may recommend an estrogen skin patch. The patch provides a low, steady supply of estrogen, which is least likely to aggravate headaches.
If hormone replacement therapy worsens your headaches, your doctor may lower the estrogen dose, change to a different form of estrogen or stop the hormone replacement therapy.



Comments
Post a Comment