Non-allergic rhinitis
Non-allergic rhinitis
Causes
Non-allergic rhinitis occurs when the lining of the inside of the nose becomes swollen and inflamed, usually because of swollen blood vessels and fluid building up in the tissues of the nose.
This swelling blocks the nasal passages and stimulates the mucus glands in the nose, resulting in the typical symptoms of a blocked or runny nose.
Some of the main causes of non-allergic rhinitis are described below.
Infection
In many cases, rhinitis develops as the result of an infection attacking the lining of the nose and throat.
This is usually a viral infection, such as a cold, but bacterial or fungal infections can occasionally cause rhinitis.
Environmental triggers
In some people, rhinitis appears to develop as a result of environmental triggers, such as:
smoke
perfume
paint fumes
changes in the weather, such as a drop in temperature
alcohol
spicy food
stress
The medical term for rhinitis caused by environmental triggers is vasomotor or autonomic rhinitis. The exact cause of this type of rhinitis is unknown, but it's believed to occur in people with very sensitive nasal blood vessels.
Medications and drugs
Rhinitis can sometimes occur as a result of using certain medications, including:
angiotensin-converting enzyme (ACE) inhibitors – a type of medication used to treat high blood pressure
beta-blockers – a type of medication used to treat various heart conditions
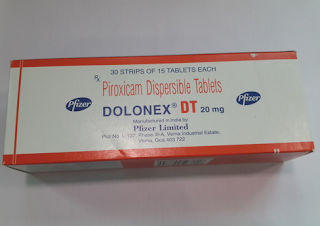
non-steroidal anti-inflammatory drugs (NSAIDs) – a type of medication commonly used to relieve pain
nasal decongestant sprays (see below)
Rhinitis can also occur as a result of drug misuse (such as cocaine).
Overuse of nasal decongestants
Nasal decongestant sprays work by reducing the swelling of the blood vessels in your nose.
However, if they're used for longer than five to seven days at a time, they can cause the lining of your nose to swell up again. This can happen even after the cold or allergy that originally caused the problem has passed.
If you use more decongestants in an attempt to reduce the swelling, it's likely to make the problem worse.
The medical term for rhinitis caused by the overuse of nasal decongestants is rhinitis medicamentosa.
Hormonal imbalance
It's thought that hormones play a role in the enlargement of the nasal blood vessels that can lead to rhinitis.
Non-allergic rhinitis can also be caused by hormonal changes due to:
pregnancy
puberty
taking hormone medication – such as hormone replacement therapy (HRT) or the contraceptive pill
Various conditions that cause a hormone imbalance in the body, such as an underactive thyroid gland (hypothyroidism), can also cause rhinitis.
Tissue damage
Inside your nose, there are three ridges of bone covered by a layer of tissue. These layers of tissue are called turbinates. A type of rhinitis called atrophic rhinitis can occur if the turbinates become damaged.
Most cases of atrophic rhinitis in the UK occur when the turbinates are damaged or removed during surgery (sometimes it's necessary to surgically remove turbinates if they're obstructing your airflow).
Turbinates play an important role in the functioning of your nose, such as keeping the inside of your nose moist and protecting the body from being infected with bacteria. If they're damaged or removed, the remaining tissue can become inflamed, crusty, and prone to infection.
Diagnosis
You should see your GP if you have symptoms of non-allergic rhinitis and the condition is affecting your quality of life.
Your GP will first ask about your symptoms. Certain symptoms, such as a cough or muscular aches and pains, would suggest that your rhinitis is caused by a viral infection.
Your GP may also ask about your medical history, as rhinitis can sometimes occur as a side effect of certain medications.
Allergy tests
If your symptoms and medical history don't suggest an obvious cause, you may need to have further tests to check if your symptoms could be caused by an allergy. This is because the symptoms of allergic rhinitis can be very similar to those of non-allergic rhinitis.
Your GP may carry out a blood test to check if you have an allergy, or they may refer you to a hospital allergy clinic for more specific tests.
One of the main tests you may have at an allergy clinic is a "skin prick test". This is where your skin is pricked with a tiny amount of a suspected allergen to see if it reacts by becoming red, raised and itchy.
If the test results suggest you don't have an allergy, you may be diagnosed with non-allergic rhinitis.
Read more about allergy tests.
Further tests
In some cases, it may be necessary to have further tests in hospital to help diagnose non-allergic rhinitis and check for any complications, such as nasal polyps or sinusitis.
Specifically, examination with an endoscope is usually necessary. This is a thin tube with a light source and video camera at one end, which is inserted up your nose and gives an excellent view of the internal part of the nose.
Other tests may include:
a nasal inspiratory flow test – where a small device is placed over your mouth and nose, and measures the air flow when you inhale through your nose
a computerised tomography (CT) scan – a type of scan that uses X-rays and a computer to create detailed images of the inside of the body
CT scans are regularly used before nasal surgery to help plan treatment.
Treatment
Treatment for non-allergic rhinitis often depends on the cause of the condition.
In some cases, such as when rhinitis is caused by a viral infection, treatment may not be necessary. This is because the infection responsible for the condition normally clears up within a week or two.
Avoiding triggers
If something specific seems to be triggering your symptoms, you may be advised to avoid possible triggers. For example, it may help to avoid exposure to smoky or polluted environments.
If your rhinitis is believed to be caused by a medication you're taking, such as beta-blockers, your GP may be able to prescribe an alternative medication to see if it helps to reduce your symptoms. Don't stop taking any prescribed medication unless advised to by a doctor.
Some cases of non-allergic rhinitis are caused by overusing nasal decongestant sprays. In these cases, the best treatment is to stop using these sprays. However, this can be difficult, particularly if you've been using them for some time.
Try not using the spray in your least congested nostril first. After seven days this nostril should open up, at which point you should try to stop using the spray in your other nostril.
It may also help to rinse your nose using a salt water solution (see below) and take antihistamine tablets that cause drowsiness to reduce night-time congestion and help you sleep.
Some specialists try to gradually switch your spray from a decongestant (which is harmful in the long term) to a steroid spray (which generally can be used for longer periods).
Cleaning the nasal passages
In many cases of non-allergic rhinitis, rinsing your nasal passages with a salt water solution can be helpful. This is known as nasal irrigation or nasal douching.
Rinsing your nasal passages helps wash away any excess mucus or irritants inside your nose, which can reduce inflammation and relieve your symptoms.
Nasal irrigation can be done using either a home-made solution or a solution made with sachets of ingredients bought from a pharmacy. Small syringes or pots (which often look like small horns or teapots) are also available to help flush the solution around the inside of your nose.
To make the solution at home, mix a teaspoon of salt and a teaspoon of bicarbonate of soda into a pint of boiled water that's been left to cool to around body temperature (don't attempt to rinse your nose while the water is still hot). To rinse your nose:
standing over a sink, cup the palm of one hand and pour a small amount of the solution into it
sniff the water into one nostril at a time – an alternative is to use a syringe to insert the solution into the nose
repeat this until your nose feels comfortable (you may not need to use all of the solution)
While you do this, some solution may pass into the throat through the back of the nose. Although the solution is harmless if swallowed, try to spit out as much of it as possible.
Nasal irrigation can be carried out several times a day and a fresh solution should be made each time.
Nasal sprays
Various types of nasal spray are available to help relieve the symptoms of non-allergic rhinitis. These include:
antihistamine nasal sprays – these help to relieve congestion and a runny nose by reducing inflammation
corticosteroid nasal sprays – like antihistamines, these work by reducing inflammation
anticholinergic nasal sprays – these reduce the amount of mucus your nose produces, which helps to relieve a runny nose
decongestant nasal sprays – these relieve congestion by reducing swelling of the blood vessels inside your nose
Many of these sprays can be bought over the counter in pharmacies without a prescription. Therefore, it's important to check the leaflet that comes with them before use, because they're not suitable for everyone. If you're at all uncertain whether you should be using one of these medications, check with your GP or pharmacist.
You should also make sure you check the manufacturer's instructions to see how to correctly use these sprays.
If you use a decongestant spray, make sure you don't use it for longer than five to seven days at a time. This is because overusing decongestants can make congestion worse.


I want to share with you all on how Dr Itua saves my life with his powerful Herbal medicines, I was diagnosed of Oral/Ovarian Cancer which i suffered from for 5 years with no positive treatment until when My son came to me in the hospital when i was laying down on my dying bed waiting for god to call out my name to join him in heaven.
ReplyDeleteMy son was so excited that very day he came across Dr Itua on Blogspot, we decided to give him a try although we Americans are so scared to trust Africans but i really have no choice that time to choose life in between so we gave a try to Dr Itua Herbal medicines, god willing he was a good man with a god gift. Dr Itua sent us the herbal medicine. It was three bottles. I take it for a three weeks instructor and these herbal medicines heal me, cure my Oral/Ovarian Cancer completely. I have been living for 9 months now with a healthy life with no more symptoms.
I'm sponsoring Dr Itua in LA Advert on Cancer patent seminar which my son will be participating too and other patent Dr Itua has cured from all kind of human disease, also if you are sick from disease like,Epilepsy,Breast Cancer,Prostate Cancer,Throat cancer,Thyroid Cancer,Uterine cancer,Fibroid,Angiopathy, Ataxia,Arthritis,Brain cancer,Hiv,. Vaginal cancer,Herpes,Colon-Rectal Cancer,Chronic Disease.Amyotrophic Lateral Sclerosis,Brain Tumor,Fibromyalgia,Fluoroquinolone Toxicity,Multiple myeloma,Tach Diseases,Leukemia,Liver cancer,
Esophageal cancer,Gallbladder cancer,,Bladder cancer,Gestational trophoblastic disease,Head and neck cancer,Hodgkin lymphoma
Intestinal cancer,Kidney cancer,Hpv,Lung cancer,Adrenal cancer.Bile duct cancer,Bone cancer,Melanoma,Mesothelioma,Neuroendocrine tumors
Non-Hodgkin lymphoma,Cervical Cancer,Oral cancer,Hepatitis,Skin cancer,Soft tissue sarcoma,Spinal cancer,Pancreatic Cancer, Stomach cancer
Testicular cancer,
Syndrome Fibrodysplasia Ossificans ProgresS sclerosis,Alzheimer's disease,Chronic Diarrhea,Copd,Parkinson,Als,Adrenocortical carcinoma Infectious mononucleosis,Vulvar cancer,Ovarian cancer,,Sinus cancer, Here Is The Wonderful Healer Contact. Name_ Doctor Itua, Email Contact: drituaherbalcenter@gmail.com, Phone/WhatsApp: +2348149277967